WORCESTER, Mass.– September 10, 2008 – To speed the pace of translating scientific discoveries into new therapies for people, two teams of researchers from Worcester Polytechnic Institute (WPI) and the University of Massachusetts Medical School (UMMS) have received grants from a cooperative pilot program to support innovative projects that blend biomedical engineering and clinical research.
Now in its second year, the grant program is funded jointly by WPI and UMMS, and is open to project teams with one or more researchers from each school. “We created this program to encourage more collaboration between our institutions, so we can leverage the strengths of each to accelerate translational research,” said Grant W. McGimpsey, PhD, associate provost for Research and Graduate Studies, ad interim, at WPI, and co-director of the UMMS-WPI grant program. “I think the two projects funded this year are not only meritorious scientifically, but they are great examples of the synergies we can achieve by working together.”
Stephen Doxsey, PhD, professor of molecular medicine at UMMS and co-director of the grant program, agreed, noting that “this program was conceived from conversations between investigators at both institutions focused on bringing more rigor to basic biological and clinical studies through the application of mathematics, modeling, engineering, optics, and physics. The proximity of two outstanding institutions with different but complementary expertise, and the enticement of funding for pilot projects, makes the program attractive to researchers from both campuses.”
One project funded this year will be directed by the team of Christopher Lambert, PhD, research associate professor in WPI’s Bioengineering Institute at Gateway Park, and Ann Rittenhouse, PhD, associate professor of physiology at UMMS. They will explore a novel approach to reconnecting brain circuits damaged by stroke. The team will use thin gold wires with bioengineered surfaces developed in Lambert’s lab to attempt linking two neurons cultured in the Rittenhouse lab. The goal is to engineer a wire that can transmit a signal from one neuron to the other, as if it were a natural connection. If successful, the team hopes the research will lead to technology for restoring electrical signals in stroke-damaged areas of the brain. They theorize such new connections would prompt remodeling of the brain to allow for rapid restoration of functions lost to the stroke. Furthermore, if they are able to establish neuronal connections and signaling with wires, the technology could be used for a variety of potential applications, including the development of motorized artificial limbs controlled by the nervous system.
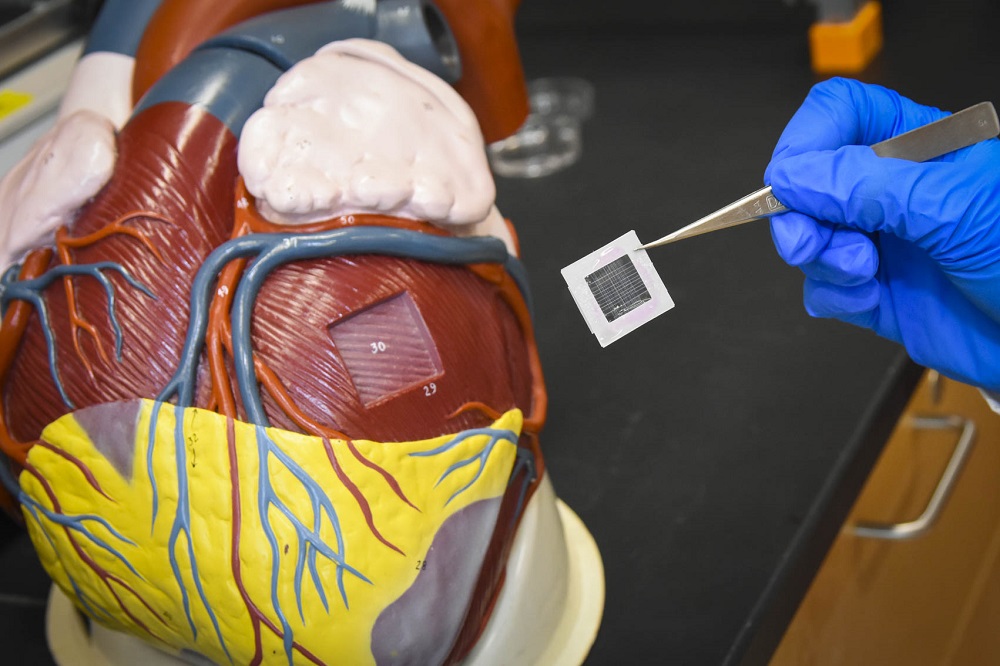
The other collaborative grant award went to the team of Marsha Rolle, PhD, assistant professor of biomedical engineering and George Pins, PhD, associate professor of biomedical engineering, both at WPI, and John Keaney, MD, professor of medicine and chief of the division of cardiovascular medicine at UMMS. This team will try to grow multi-layered sections of human blood vessel tissue in the lab. The work could lead to an effective way to generate replacement blood vessels for transplantation, and could establish a better model system for studying cardiovascular disease.
The team will use customized co-culture devices designed in the Pins lab and fabricated by the machine shop at WPI. The devices anchor scaffolds made of collagen (or other structural proteins) in test wells, with different cells applied to each side of the scaffold. The team will grow human smooth muscle cells on one side of the collagen, then seed the other side with human endothelial cells, which are the cells that line the inside of blood vessels. Rolle’s lab will use genetic tools to engineer the smooth muscle cells to grow in ways that may allow them to function more like their counterparts in naturally occurring blood vessels. Keaney’s lab will closely examine the endothelial cells during the development process, to see how they behave and react in the model system. In the body, smooth muscle and endothelial cells are in constant communication, sending signals that regulate blood vessel function. This program hopes to approximate the natural architecture of blood vessels so that more can be learned about how the various layers of cells interact, both in a healthy state and when disease arises.
“Bringing together WPI’s strengths in engineering and applied research, with the basic and clinical science excellence at UMass, is a logical fit,” McGimpsey said. “Early seed money for research like this is critical for testing ideas, seeing what works, and gathering data that can then be used to launch major research and development efforts with external funding. That’s the hope for our collaboration with UMass.”
With the second round of grants now awarded, Doxsey said he hopes the WPI-UMMS program will continue to grow and foster important translational research. “There is great excitement about the potential of the joint research endeavors established through the UMMS-WPI funding initiative,” Doxsey said. “Not only does this financial support provide opportunities to establish new institutional and individual partnerships, and to develop new marketable lead products for industry, but there is hope that these efforts will help crack difficult problems in biology and disease, and facilitate translation of those successes into the clinic.”
About UMass Medical School
The University of Massachusetts Medical School, one of the fastest growing academic health centers in the country, has built a reputation as a world-class research institution, consistently producing noteworthy advances in clinical and basic research. The Medical School attracts more than $176 million in research funding annually, 80 percent of which comes from federal funding sources. The work of UMMS researcher Craig Mello, PhD, an investigator of the prestigious Howard Hughes Medical Institute (HHMI), and his colleague Andrew Fire, PhD, then of the Carnegie Institution of Washington, toward the discovery of RNA interference was awarded the 2006 Nobel Prize in Physiology or Medicine, hailed as the "Breakthrough of the Year" in 2002 by Science magazine and has spawned a new and promising field of research, the global impact of which may prove astounding. UMMS is the academic partner of UMass Memorial Health Care, the largest health care provider in Central Massachusetts. For more information, visit www.umassmed.edu.