Development of new therapies for a range of medical conditions—from common sports injuries to heart attacks—will be supported by a new production-scale microthread extruder designed and built by a team of graduate students and biomedical engineering faculty at Worcester Polytechnic Institute (WPI).
The new microthread extrusion system is in the final stages of testing and validation, and will soon be manufacturing thousands of hair-like biopolymer threads a day at WPI's Life Sciences and Bioengineering Center at Gateway Park.
Threads of Hope
WPI team develops biopolymer microthreads for tissue regeneration, wound healing, and cell therapy applications.
"The use of these microthreads is spreading across labs here at WPI, and to our collaborators around the country," said Glenn Gaudette, associate professor of biomedical engineering at WPI, who oversaw the development of the new extrusion system. "So we needed greater quantities of the microthreads and a system to standardize and control the production process."
The idea for using microthreads as a basis for tissue engineering was developed in the laboratory of George Pins, associate professor of biomedical engineering at WPI, who was looking for a better way to repair the anterior cruciate ligament (ACL) in the knee. The current surgical treatment for ACL tears or ruptures, which affect an estimated 100,000 people in the United States each year, involves removing a section of healthy tendon from another part of the body and grafting it into the knee to replace the ACL. While surgery is often required to help patients regain full use of the knee, the current approach is not considered ideal because it injures one part of the body to repair another.
"The ACL, like other ligaments and tendons, is a fibrous cable-like structure," Pins said. “So the original idea was to use thin collagen threads, bundled into cables that mimic the natural structures in the body, as a scaffold for the tissue engineering that would be used to replace the ACL."
Collagen is the main structural protein of the body. It’s the building block for skin and connective tissues such as tendons, ligaments, muscle, and cartilage. So Pins and his lab team theorized that thin threads of collagen would be well-tolerated by the body. As the work continued, the team also began making microthreads from fibrin, which is the main protein in blood clots; since clotting is an early response to injury Pins believed that fibrin threads could become useful scaffolds for wound-healing applications.
Initially, Pins and his lab team made each thread by hand, using a large syringe to push out a bead of collagen or fibrin, draw it into a bath of solution, then lift it out by hand to dry suspended over the edges of a cardboard box. "I always looked for the student with the steadiest hands to draw out the threads," Pins said, noting that it was difficult to get the threads to be consistent in diameter and length.
While the hand-drawn method demonstrated the promise of the concept, Pins challenged several of his undergraduate students to develop an automated system for making the threads in a consistent manner. Two Major Qualifying Project (MQP) teams tackled the challenge over the course of two years. Working collaboratively with WPI faculty members in mechanical engineering and robotics engineering, they developed a working bench-scale prototype that automated most of the thread production process. "The prototype worked well, and produced more consistent threads," Pins noted.
By early 2010, interest in the microthreads had expanded beyond Pins's lab, as colleagues at WPI saw opportunities to use them in their own areas of research. With demand for new threads growing, Paul Vasiliadis, a member of one of the MQP teams, began planning to take microthread production to the next level. After earning his bachelor's degree in 2010, Vasiliadis joined Gaudette's lab as a graduate student and became the lead developer of the production-scale extrusion system now being commissioned. Computer-controlled, the new system is capable of continuous extrusion with a range of specified thread diameters and quantities.
"I think this project shows the importance of bringing together multidisciplinary teams, focused on the biology and the engineering, to create solutions that will meet real clinical needs," Gaudette said.
The Pins lab continues to develop the microthread technology for use as potential ligament and tendon scaffolds while also working to optimize the composition and mechanical properties of the threads. For example, they are experimenting with ways to control the tensile strength of the threads, and to control the rate at which the threads dissolve once implanted in the body. They have also developed new technologies to tailor the surface topographies and biochemistries of the microthreads to provide specific signaling cues that they predict will direct cell-mediated tissue responses.
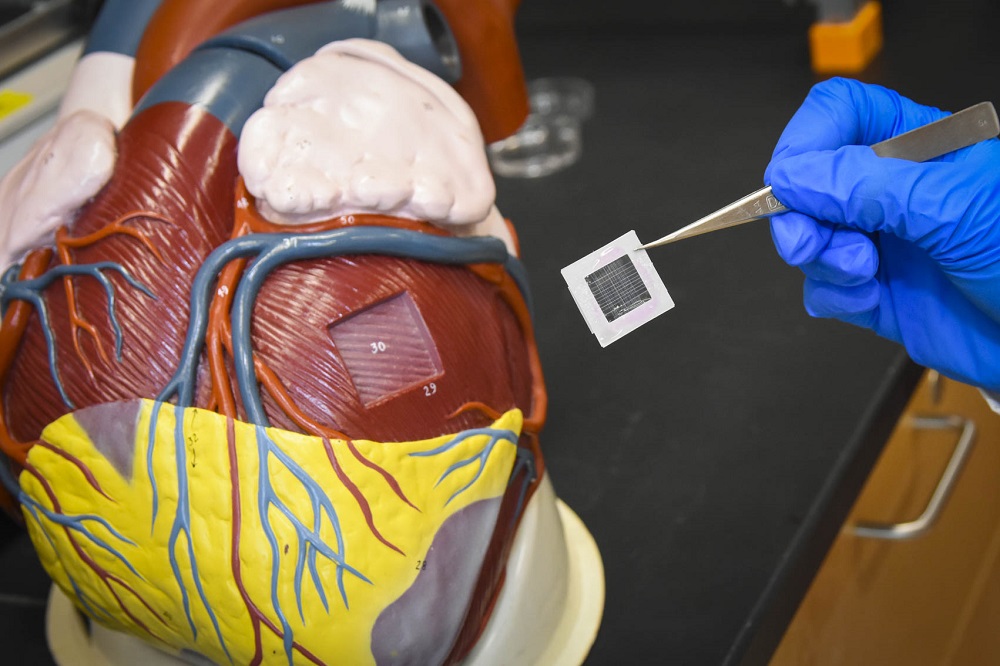
In Gaudette's lab, the threads are being used as biological sutures to deliver bone marrow–derived adult stem cells known as human mesenchymal stem cells (hMSCs) to cardiac tissue damaged by disease or trauma. Studies by Gaudette and others have shown that when hMSCs are delivered to damaged hearts, they moderately improve cardiac function. A major challenge in these studies, however, is getting sufficient numbers of hMSCs to engraft into the damaged heart tissue. Prior methods of injecting the cells into the bloodstream, or directly into the heart muscle, yielded low results, with 15 percent or fewer of the cells injected actually surviving and attaching to the heart muscle. Using the microthreads to deliver cells to the heart has changed that dynamic.
"The early studies are very promising," Gaudette said. "We have developed ways to seed and grow the stem cells on the microthreads, and deliver them directly to the area needed, with more than 60 percent of those cells successfully engrafting. That’s a major improvement."
Other researchers at WPI are using fibrin-based microthreads as a platform to restore muscle tissue that was damaged by traumatic injury. In those studies, the microthreads do double duty: they are seeded with new cells that could regenerate muscle tissue, and they serve as a muscle-like scaffold to promote the body's own healing and regenerative processes.
"This is becoming a platform technology, growing in ways we hadn't imagined when we first began this line of research," Pins said. "It's exciting to see the clinical potential for this technology accelerating. And, as an educator, it's gratifying to know how fundamentally important the students' contributions have been to this work."
With testing, validation, and operator training now under way, the new extrusion system is expected to be supplying WPI labs with research-grade microthreads later this spring.