Early detection of blood loss to save the lives of soldiers wounded on the battlefield is the goal of a three-year research and development project to be launched this fall at Worcester Polytechnic Institute (WPI). Funded by a $1.9 million grant from the U.S. Army, the research will be conducted in collaboration with the University of Massachusetts Medical School (UMMS).
The project will be led by Ki Chon, PhD, professor and head of WPI’s Biomedical Engineering Department, and Yitzhak Mendelson, PhD, associate professor of biomedical engineering. The WPI team will develop miniaturized wireless sensors that soldiers can wear into battle. They will also create the mathematical algorithms needed to process signals from those sensors to simultaneously measure seven physiological parameters, including a novel way to detect bleeding. In addition to sensors worn on the body, the WPI team will place the same monitoring capabilities on smartphones, which Army medics can use as hand-held diagnostic tools. Both the wearable sensor and smartphone technologies will be evaluated at the medical school in an observational study of trauma patients directed by Chad Darling, M.D., assistant professor of emergency medicine, and David McManus, M.D., assistant professor of medicine.
"We have a responsibility as a country to ensure that our soldiers have the best possible technology keeping them safe and alive on the battlefield," said U. S. Rep. Jim McGovern (D-MA). "This highly-competitive federal grant award is recognition of the groundbreaking research being conducted at WPI to develop innovative technologies to protect the men and women in our armed services. Additionally, the vital role UMass Medical School is playing in the program is further evidence of the great cross-institution partnerships among the universities in Massachusetts that so often lead to important advances."
In the new project, Chon’s laboratory will focus on signal processing and adapting the technology for use on a smartphone, while Mendelson’s team will lead the wearable sensor device development. The teams have collaborated in the past, and have developed sensor systems and signal processing algorithms for other applications. "This is an ambitious project, and we are pleased that the U.S. Army has seen merit in our proposal," Chon said.
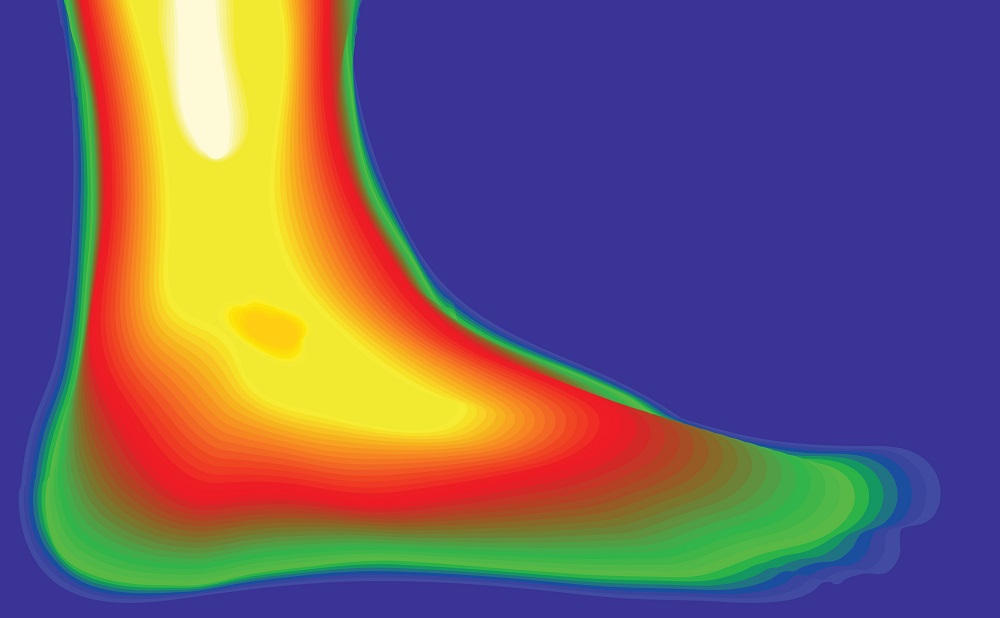
The monitoring system to be developed will use light to measure vital signs. Small sensors will shine infrared and visible light through the skin and detect how different frequencies of light are absorbed by pulsing arterial blood. A series of algorithms will correlate subtle shifts in the spectra to a wide range of physiological parameters. On the smartphone platform, the built-in video camera will provide the light and record the reflections. It is the same basic technology used in pulse oximeters, those now-familiar devices that clip on a patient’s finger to measure blood oxygen levels. Chon and Mendelson’s approach, however, takes the technology to a far more sophisticated level.
In earlier work, Chon and Mendelson developed wireless sensor hardware and signal processing algorithms that successfully measured heart rate, heart rhythm, respiration rate, skin perfusion, and blood oxygen saturation. Early proof-of-concept studies on healthy patients donating blood has recently shown that a light-based sensor system can also detect early signs of a reduction in blood volume in the body using an algorithm Chon developed. The team speculates that the same algorithm may be able to detect dehydration in patients not suffering from blood loss.
Through the Army program, the WPI team will continue hardware, software, and algorithm development with the aim of optimizing the sensors’ size, durability and accuracy. They will also evaluate where best to place sensors on the body, and test varying system configurations using multiple sensors to analyze physiological signals from different parts of the body simultaneously. The sensors will also include embedded accelerometers to measure body movement and posture, and a wireless link that will allow a medic to monitor the health of soldiers and react with emergency aid as needed.
Among the biggest challenges of sensor development for battlefield conditions is maintaining accurate measurements while soldiers are moving. Motion artifact contamination, interference caused by body movements, degrades the quality of the signals being measured and leads to erroneous readings. "This is not a trivial matter, so we hope that our strategies will work to overcome this noise," Mendelson said. "Unless we can prove that the information is consistently accurate and reliable, medics and trauma physicians won’t trust or use the device."
Beginning in the second year of the project, prototypes developed at WPI will be used by the UMass Memorial Medical Center’s emergency department to monitor trauma patients’ vital signs and detect blood loss. Severely injured patients, usually accident victims, will be monitored as they are transported by the medical center’s Life-Flight helicopter. Other patients will be monitored when they arrive in the center’s emergency room by ambulance, using both wearable sensors and the smartphone application. In addition, the UMMS clinical team will help develop decision support tools to be embedded in the smartphone. When the monitoring system is deployed in the field, those tools will respond as vital signs are measured and prompt a medic or first-responder with information to guide treatment.
"This is a very exciting program, and we’re pleased to be able to work with the WPI team," Dr. Darling of UMMS said. "The majority of trauma victims we see have a blunt-force injury, with no visible signs of bleeding. So we are always concerned about internal bleeding, and typically order a CT scan to see what’s happening inside. An early-detection system for internal bleeding would be helpful, and certainly would be very important for first-responders in the field."
Dr. McManus said that the UMMS clinical research team has designed an ambitious study that will monitor trauma patients in the field, and follow them through the emergency department and on to surgery or intensive care as their treatment dictates. The new WPI systems will not be used to make medical decisions during this phase of development. As qualifying trauma patients undergo diagnosis and treatment, research coordinators will use the prototypes to monitor patients and capture data. The corresponding sensor data will then be analyzed and correlated with the clinical data the trauma team recorded and used to determine the actual extent of blood loss.
"Having the opportunity to collaborate with the trauma team at UMass Medical is extremely important for our work," Mendelson said. "Their clinical understanding and experience will help us refine the technology."