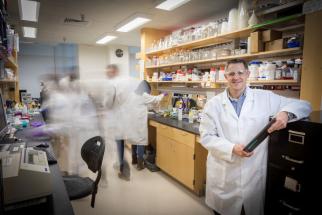
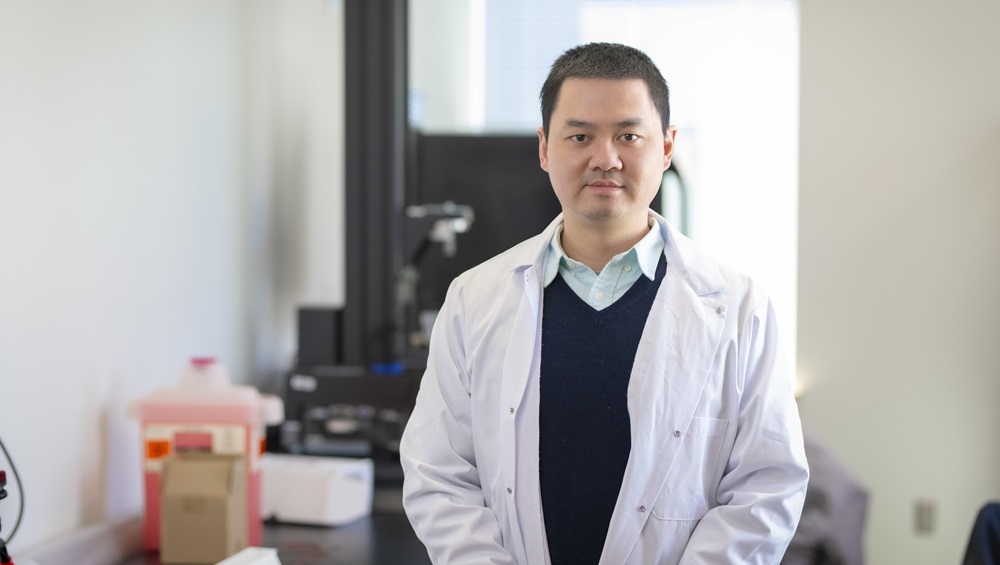
WPI Researcher Kristen Billiar has been awarded $429,456 from the National Institutes of Health to investigate how stretching and blood flow can inhibit or encourage cardiovascular cells to populate and grow in tissue-engineered heart valves.
The three-year project focuses on experimental valves that are not yet used in humans, and the work will expand understanding about how mechanical forces propel cells in the body.
“Existing heart valves have drawbacks, and there is hope that future valves made of engineered materials could be surgically implanted and become populated with a patient’s own cardiovascular cells,” said Billiar, professor and head of the Department of Biomedical Engineering. “For that to happen, we need to know more about how or why cells populate a heart valve and whether there is anything that can be done to help those cells attach to and grow on a scaffold that is shaped like a valve.”
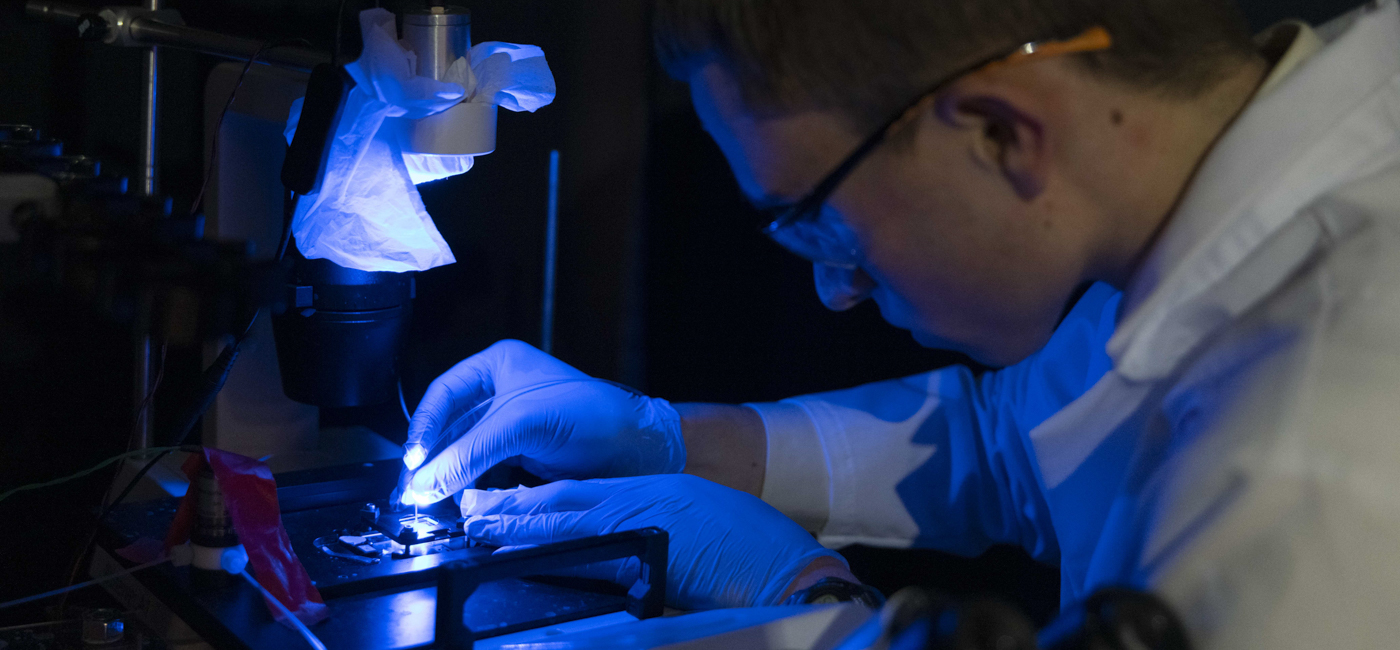
Billiar will lead microfluidic laboratory experiments that will stretch tiny amounts of biopolymer materials and expose them to fluid flows to examine how cells attach, proliferate, and migrate. A total of 18 undergraduate students will be involved in the project by refining the design of test systems and working on experiments.
“The students will learn hands-on research skills, work with state-of-the-art equipment, and play a critical role in the success of this project,” Billiar said.
The project builds on Billiar’s previous work, which has examined how cell death leads to calcium deposits in heart tissue that cause aortic valves to fail and how mechanical forces and stresses affect programmed cell death.
The human heart has four valves that control blood flow through four chambers. The most commonly replaced valve is the aortic valve, which opens and closes to control the flow of blood from the heart’s lower left chamber into the aorta, the body’s primary artery.
In adults, the aortic valve can be damaged by disease. Babies may also be born with improperly formed aortic valves.
When valves cannot be surgically repaired, doctors may replace a damaged valve with a mechanical valve made of durable materials such as carbon, or a valve made from animal or human heart tissue. Both types of valves, however, have limitations: Patients with mechanical valves must take blood thinners regularly to avoid clotting problems, and valves made from living tissue break down over time. More than 200,000 heart valves are replaced worldwide every year.
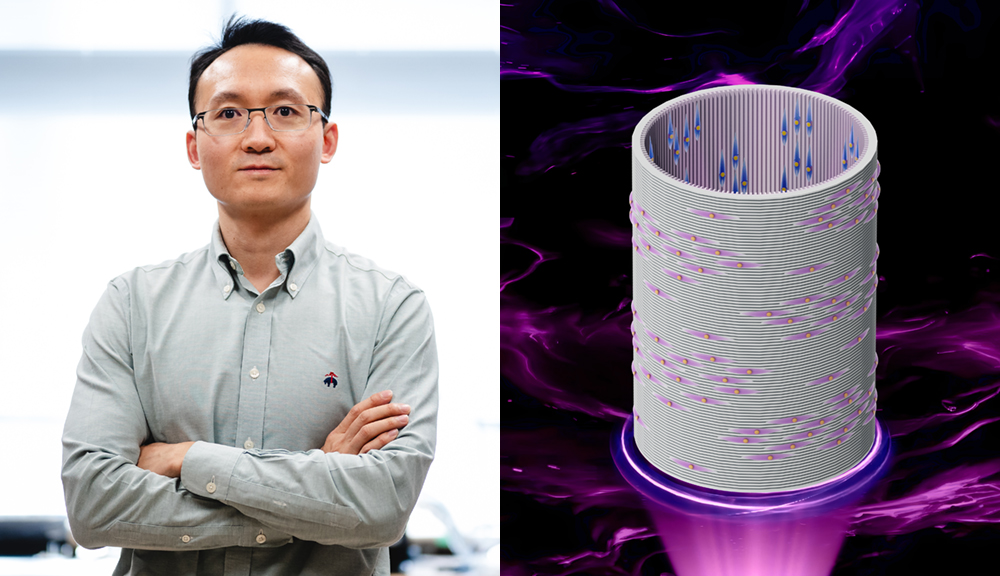
Experimental technologies involve using materials such polymers, similar to those used in absorbable surgical sutures, or biopolymers such as collagen, to build scaffolds that could be implanted in a heart valve. Over time, the body’s heart cells would grow a new living valve on the scaffold.
Although Billiar’s project focuses on heart valves, he said a better understanding of how stretch and flow impact cells could lead to advances in other fields, as well.
“Cancer and wound healing occur in moving tissues, too,” Billiar said. “My lab group hopes that our work will encourage researchers to adopt dynamic, moving methods to study how cells move, grow, and differentiate into other types of cells in the body.”