With the guidance of WPI’s Medical Advisory Board, the university has used science and mathematical models to shape strategies for keeping the campus safe and preventing the spread of COVID-19, while at the same time, faculty members are doing research to help in the global fight against the coronavirus pandemic.
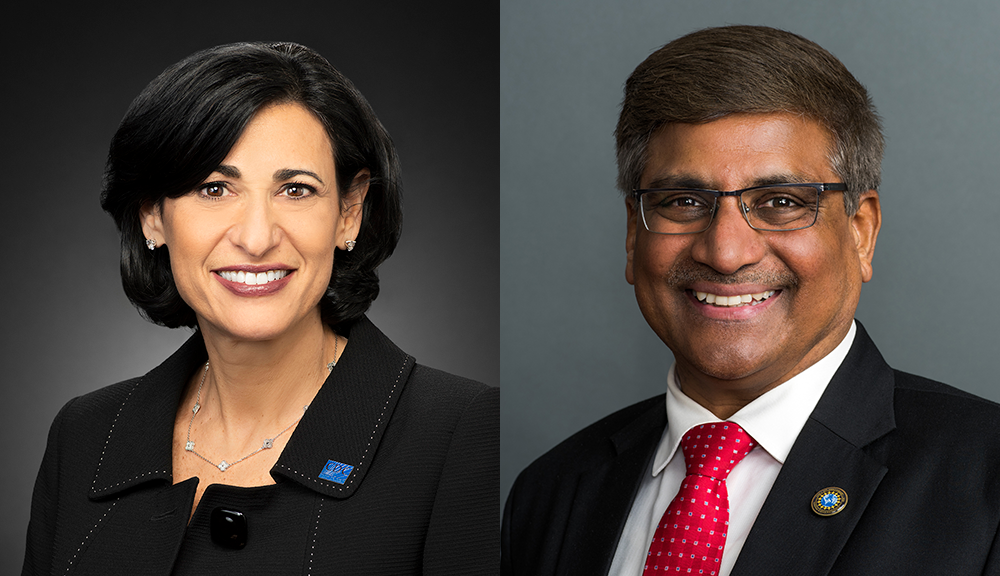
The Critical Conversations panel, WPI’s COVID Response: Science and Innovation, held Dec. 2, featured Rochelle Walensky, M.D., chief of infectious diseases at Mass. General Hospital, and a member WPI’s Medical Advisory Board; today she was named president-elect Joe Biden’s choice as the next director of the Centers for Disease Control and Prevention.
With her pending appointment to head the CDC, Walensky will succeed Robert Redfield; she will assume a critical role in helping the Biden administration rein in the coronavirus pandemic.
Panelists from WPI’s faculty outlined their current research and how it could be used by the medical community in COVID diagnosis and treatment.

The Medical Advisory Board provides expertise, scientific and medical insight, and advice as the university manages the health challenges associated with COVID-19. Since July, members of the board have met (via Zoom) with President Leshin and other senior leaders to inform the critical work being done by the university’s Coronavirus Emergency Response Team (CERT). In addition to guiding isolation and quarantine plans, the group helped address several questions about physical spaces on campus.
While many colleges and universities around the country have sent students home and shifted to totally remote learning, the measures WPI has taken have allowed the university to continue in-person, hybrid, and remote learning; to move forward with research; to maintain residential status; and to facilitate employees working both on campus and remotely.
“As a member of the university’s Medical Advisory Board, Dr. Walensky’s expertise and advice have been invaluable to WPI’s successful management of this pandemic to date,” said WPI President Laurie Leshin. “The entire WPI community is deeply grateful to her, and I’m thrilled that president-elect Biden has appointed her as the next director of the CDC. The nation will be better off with this brilliant woman at the helm.”
The Critical Conversations discussion was moderated by Jean King, Peterson Family Dean of Arts & Sciences, neuroscientist and biomedical researcher, and a member of WPI’s Medical Advisory Board.
“At WPI, we have use science, medicine, innovation and constant surveillance (from CERT) to keep us safe,” King said. “We have to keep vigilant and stay informed.”
In addition to Walensky, the panel included:
- Dmitry Korkin, professor computer science—Korkin and a team of graduate students used molecular modeling to reconstruct the 3D structure of major viral proteins and their interactions with human proteins, a structural genomics map of the coronavirus that has been made available to researchers and anyone else worldwide.
- Reeta Rao, associate dean of graduate studies and professor of biology and biotechnology—Rao’s research program focuses on understanding and managing fungal infectious diseases. She also has appointments at UMass Medical Center and the Broad Institute.
- Haichong Zhang, assistant professor robotics and biomedical engineering—Zhang is using a National Institutes of Health grant to build a robotic ultrasound machine to detect disease symptoms in the lungs, a significant development that will allow healthcare providers to minimize their exposure to the virus when conducting assessments of COVID-19 patients.
- Andrea Arnold, assistant professor mathematical sciences—her work in mathematical modeling and data simulation techniques can be used to analyze real world problems, including the spread of infectious diseases. Forecast predictions can be made in the number of projected cases of hospitalization, which can then be used to help inform decision making and help the CDC and its partners respond to the COVID-19 pandemic in planning, resource allocation, and implementation of social distancing measures.
- Ulkuhan Guler, assistant professor electrical and computer engineering—Guler is developing a miniaturized wireless oxygen sensor that would enable infants to leave the hospital and still be safely monitored from home. Work on a miniaturized oxygen sensor is under way—Guler and her students have already created a chip for the device, and work has begun on thin, flexible sensors needed for the wearable version.
In response to a question from King, Walensky said she became an infectious diseases specialist after interning in Baltimore. During that time in the mid-1990s, a combination drug treatment known as the “AIDS cocktail” was introduced and approved by the FDA. Until that time nearly everyone who contracted AIDS died, she said, and the cocktail gave the first hope to AIDS sufferers. “I decided to be an infectious disease specialist,” she said. “I thought then that AIDS would be the only pandemic I’d see.”
Walensky said the rapid development of a number of COVID vaccines simultaneously has been an incredible story of success. “The fastest vaccine had previously taken four years to develop … the fact of having 90 percent efficacy is outstanding. We’ve never had mRNA (messenger RNA) vaccines before. Getting doses to everyone will be a challenge we’ve never had.”
She added that there are likely to be a few side effects from the COVID vaccines, with 50 to 60 percent of recipients showing symptoms. “There will be fevers, head and muscle aches, chills,” she said. “We should not be deterred and must get the second dose” of the two-part inoculation.
Walensky said that the pandemic has shone a light on the vulnerable and made the question of who gets the COVID vaccine front and center for public health officials. She pointed out that at the state level—at Mass General and other hospitals—working out plans so that critical employees are vaccinated. “It’s not just the nurses and doctors. Unit clerks, food services, anyone who walks into the ICU” will be vaccinated, she said.
“We need to be communicating. It’s easy for me to say, ’I’ll take the vaccine.’ But to people who live in more vulnerable communities—who for decades have been ostracized, who have not been supported in their health care—now we’re saying. ‘trust us, we’ll support you now.’ That’s a really hard message. I’m not sure it will be well received. We have a lot of work ahead of us to regain the trust of some of these communities. I don’t think we should minimize what that’s going to take.”
-Martin Luttrell