Among the important features the algorithm focused on were the number of drains used during the surgery, the amount of postoperative bleeding, and the number of days until the patient was able to resume a regular diet. “Pancreatic cancer is a very difficult disease to treat,” she says, “so it is helpful for physicians to have this data-inferred knowledge as they develop treatment plans for their patients.”
Using similar approaches, Ruiz and her team are mining data from patients with sleep disorders, searching for patterns and identifying features that could lead to improved treatments. In an ongoing partnership with neurologists at UMMS, she has established a structured database that currently contains the medical records of 1,000 sleep disorder patients — about half a gigabyte of data for each patient. “One sleep study records data from 55 sensors worn by the patient for the entire night’s sleep, which generate an enormous amount of data,” she notes.
Unlike the pancreatic surgery project, which sought to answer a specific question, the sleep data mining project is open-ended and “unsupervised,” she says. Her research group has developed techniques that are able to automatically discover patterns across a wide spectrum of patient data: patterns that relate demographic information, medical history, family history of disease, exercise habits, drinking and smoking habits, biomedical signals, medical treatments, and medications. “In this case, we did not tell the algorithm how to organize the data,” she says, “because we didn’t want to bias it and prevent it from discovering novel patterns on its own. If we knew what the important patterns were, we wouldn’t need machine learning.”
Using these unsupervised techniques, Ruiz’s group has discovered novel patient subpopulations that exhibit distinct medical and behavioral properties. “By analyzing the subpopulations uncovered by our algorithm,” she says, “we determined that they can be characterized by their dynamic sleep properties — high vs. low efficiency — and that static properties, including age, collar size, smoking frequency, heart disease, and BMI [body mass index], differ across these populations in a statistically significant manner.”
The project is ongoing. Ruiz says she expects that many other medically meaningful patterns will be uncovered that will shed light on the nature and treatment of sleep disorders.
Translating Data for Patients
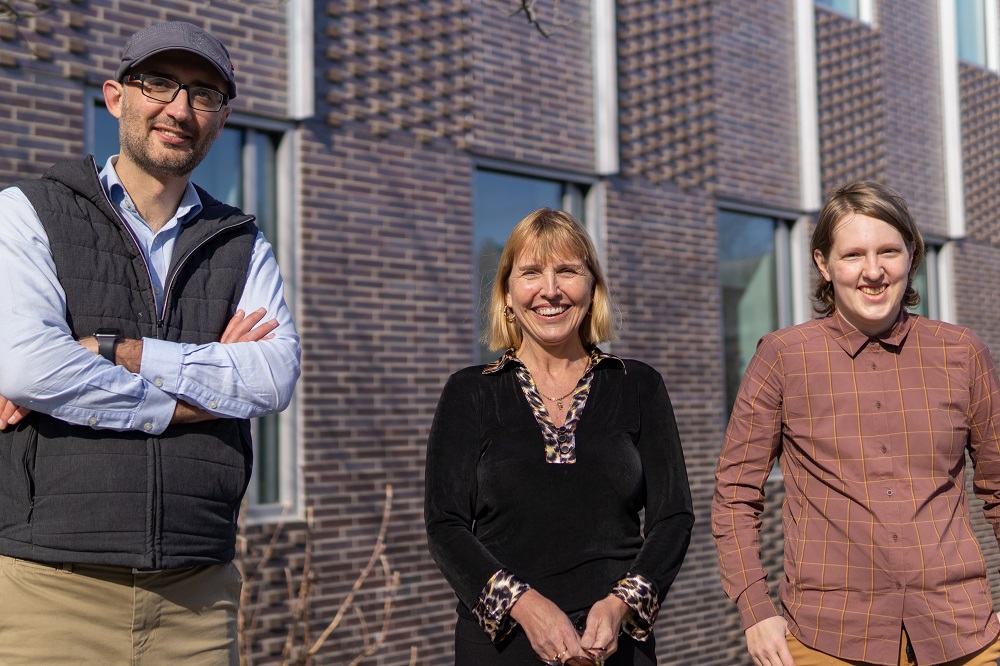
In WPI’s Foisie Business School, professor Diane Strong, PhD (at left, above), and associate professor Bengisu Tulu, PhD, are leading several teams developing smartphone-based applications that extend the impact of knowledge gleaned from digital health data.
“All the apps you see on the market today are trackers: tracking physical activity, tracking what you eat,” Tulu says. “With our apps, tracking is just the start.”
Tulu and Strong partner with clinicians and researchers at UMMS to embed evidence-based medical guidance in their apps to provide users with clinically sound prompts and action items. “In our view, a health app has to do more than tell you your numbers,” Strong says. “It should also be able to give you evidence-based information that will help you manage your own care.”
Among the smartphone apps developed by the WPI teams, which include several other WPI faculty members and students (graduate and undergraduate), is Sugar, which helps people with type 2 diabetes control their blood glucose levels and monitor severe foot ulcers, and RELAX, which helps people lose weight and overcome stress. Both are in early clinical testing with patients at UMMC.
One of the latest apps leverages a national database managed by UMMS on outcomes of total joint replacement surgeries. Patients will track their pain levels and other metrics on a daily basis using their smartphones. When they come to the clinic, the app will summarize their data and relate it to cases in the database, to give the clinician better information to assess progress and plan treatment. The app will soon be tested with UMMC patients.