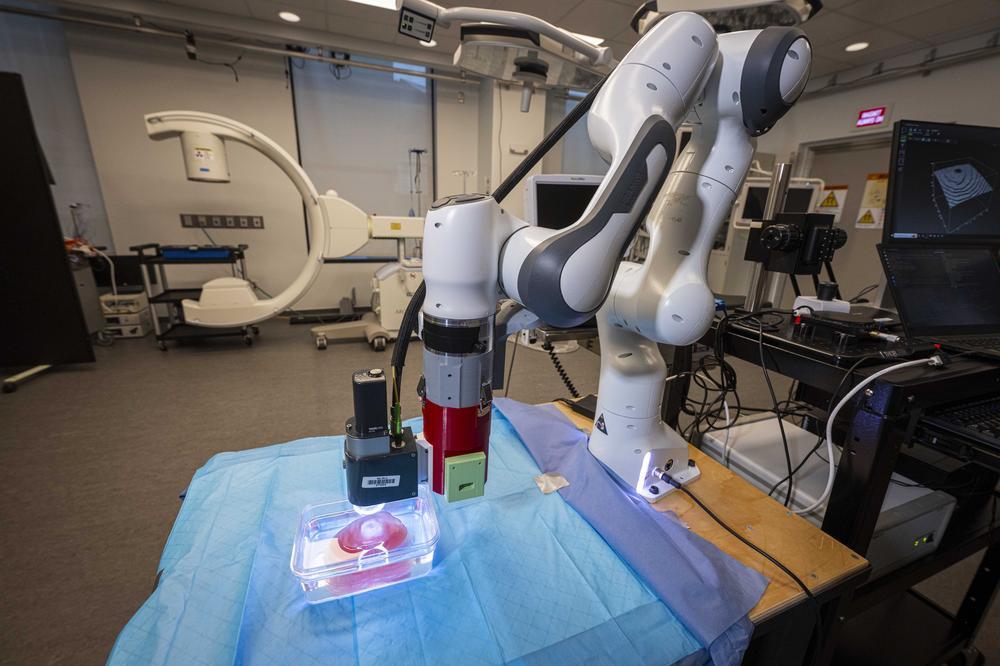
A novel robotic system may help transform the detection of prostate cancer, the last form of cancer still diagnosed with blind needle biopsies. The heart of the system is a specially designed MRI-compatible robot that can work inside the bore of an MRI scanner to help a physician guide a biopsy needle precisely toward a target of interest identified using real-time images. It promises to make prostate cancer biopsies faster, more accurate, less costly, and less discomforting for the patient.
The robotic system was developed by a team of WPI robotics engineers led by Gregory Fischer, PhD, associate professor of mechanical engineering and robotics engineering and director of WPI’s Automation and Interventional Medicine (AIM) Laboratory. The work has been carried out in collaboration with researchers at Johns Hopkins University, Brigham and Women’s Hospital in Boston, and Acoustic MedSystems Inc.
The system is currently being tested as part of a larger clinical research program at Brigham and Women’s funded by a Bioengineering Research Partnership award from the National Institutes of Health through the National Cancer Institute. The program aims to replace blind needle biopsies with image-guided technology, notes Clare Tempany, MD, professor of radiology at Harvard Medical School, chair of research radiology at Brigham and Women’s, and principal investigator for the research program. “The ultimate goal of our group is to develop enabling technologies that extend the capabilities of physicians to treat their patients.”
Most prostate biopsies today are performed with the aid of ultrasound, which can localize the prostate but not readily detect potential cancers. Requiring multiple needle insertions, the biopsies suffer from low sensitivity and often misleading results. In fact, about 35 percent of serious tumors may be missed during initial biopsies.

 Gregory Fischer, second from right, with PhD candidates, from left,
Gregory Fischer, second from right, with PhD candidates, from left,