Worcester Polytechnic Institute (WPI) will lead a five-year study to determine whether artificial intelligence can help doctors steer people dealing with chronic pain away from potentially addictive opioids and toward mindfulness-based approaches.
The new National Institutes of Health (NIH) HEAL (Helping to End Addiction Long-term) initiative-funded study will employ machine learning, a form of artificial intelligence, to look for clues in patient data that could help doctors better determine who is likely to benefit the most from mindfulness-based stress reduction, or MBSR, in managing their pain.
“For physicians, it will be a new day,” said Jean King, the Peterson Family Dean of Arts and Sciences at WPI. “To be able to predict who would respond well to non-pharmacological interventions will truly save lives.”
WPI has received $1.6 million in NIH funding to start designing the trial; if the team’s defined benchmarks are met, the research team and the university could receive a total of nearly $9 million in research funding over the course of the next five years.
The findings of the study could give healthcare providers powerful tools to help people avoid taking opioids that can lead to lifelong struggles with addiction. Over-reliance on opioids for pain management can have devastating consequences; in 2021, more than 16,000 people died from prescription-opioid-related overdoses, and more than 80,000 people died from overall opioid-related overdoses, one death every 6 minutes. There have been concerning increases in opioid-related deaths in Black and Native American populations.
At the same time, chronic pain is also a major concern. A recent U.S. Centers for Disease Control and Prevention Morbidity and Mortality Report estimated that more than 51 million people–more than 20% of U.S. adults–have chronic pain.

Previous studies have found that MBSR is effective in helping people deal with chronic pain, but the mindfulness-based approach does not work for everyone, and doctors and clinicians don’t know exactly for whom it would work and why.
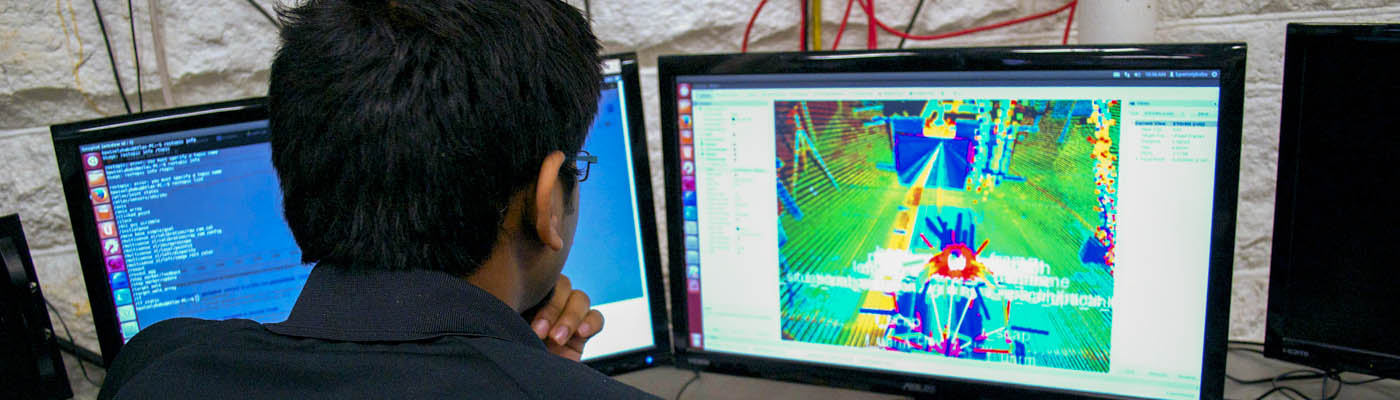
Focusing specifically on chronic lower back pain in diverse populations, the study will glean physiological data such as sleep patterns, heart rate, and general physical activity collected via fitness sensors worn by 350 participants during a six-month trial. Combined with self-reported information on depression, anxiety, pain, and levels of social support, the data will be analyzed by custom-designed machine learning models to detect patterns that might be impossible for a doctor to notice. The information will allow the model to predict whether a patient would beneficially respond to mindfulness, helping doctors better tailor treatments for individual patients.
That predictive power could prove to be a powerful tool for physicians who previously may have been wary of prescribing mindfulness-based stress reduction, said Carolina Ruiz, the WPI Associate Dean of Arts and Sciences and Harold L. Jurist ’61 and Heather E. Jurist Dean’s Professor of Computer Science, who has been involved in researching and teaching machine learning for more than two decades. She added that the machine learning model used in the study will be interpretable–doctors and researchers will be able to pinpoint exactly why a patient may or may not respond well to mindfulness methods.
“It will save time for the patient—they won’t have to go through a treatment that isn’t going to help,” she said. “It will also save a lot in healthcare costs and could be applicable to other types of pain and other types of treatment.”
The study, dubbed Integrative Mindfulness-based Predictive Approach for Chronic low back pain Treatment, or IMPACT, will bring together a diverse group of researchers at WPI, UMass Chan Medical School, and Boston University Chobanian & Avedisian School of Medicine. Along with King and Ruiz, WPI faculty researchers include Emmanuel Agu, the Harold L. Jurist ’61 and Heather E. Jurist Dean’s Professor of Computer Science and MPI, Angela Incollingo Rodriguez, assistant professor of psychological and cognitive sciences, Zheyang Wu, professor, mathematical sciences, and Benjamin Nephew, assistant research professor, biology and biotechnology.